-

Presented by: Mr Harry Petrushkin (Consultant Ophthalmologist, Moorfields Eye Hospital, London)
Learning Objectives
An overview of established and emerging synthetic and advanced treatments for inflammatory eye disease, including: -topical -intra-orbital -synthetic oral -biologics and biosimilars -small molecule therapies Bridging perceived clinical barriers to cross specialty prescribing. Non-doctor professionals prescribing medications for uveitis Structured screening clinics run by advanced pharmacists at Moorfields Eye Hospital. Local therapy with biologic by non-doctors healthcare professionals. -
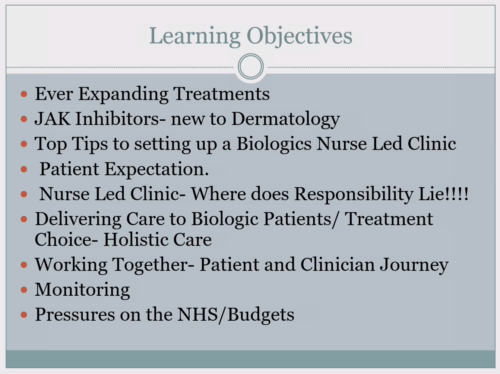
 Presented by: Teena Mackenzie (Advanced Nurse Practitioner, Royal Berkshire Hospital, Reading)
Presented by: Teena Mackenzie (Advanced Nurse Practitioner, Royal Berkshire Hospital, Reading)Learning Objectives:
Describe the ever expanding treatments in inflammatory dermatology. JAK inhibitor use in dermatology. Top tips to setting up a biologics nurse led clinic. Managing patient expectation. Nurse led clinic: where does responsibility lie. Delivering care to biologic patients. Treatment choice and holistic care. Working together: Patient and clinician journeys. Monitoring medications in dermatology. Pressures on the NHS and budgets. -

 Presented by: Dr Deepak Jadon
Presented by: Dr Deepak JadonLearning Objectives
Clinical overview of psoriatic arthritis (PsA) and rheumatoid arthritis (RA). Update on advanced therapies for PsA and RA. British Society of Rheumatology guidelines for DMARD use in pregnancy. Multi-speciality models of care. The benefits of multi-speciality meetings. -

 Presented by: Teena Mackenzie (Advanced Nurse Practitioner, Royal Berkshire Hospital, Reading)
Presented by: Teena Mackenzie (Advanced Nurse Practitioner, Royal Berkshire Hospital, Reading)Learning Objectives
Emerging biologic and small molecule therapies for Crohn’s disease. Emerging biologic and small molecule therapies for ulcerative colitis. Safety of these emerging treatments. The gastrointestinal microbiome. Future treatment for inflammatory bowel disease. Considerations when co-managing patients with inflammatory bowel disease, arthritis, skin and/or eye disease. -
 Presented by: Mr William Gregory (Consultant Physiotherapist, Salford Royal Hospital)
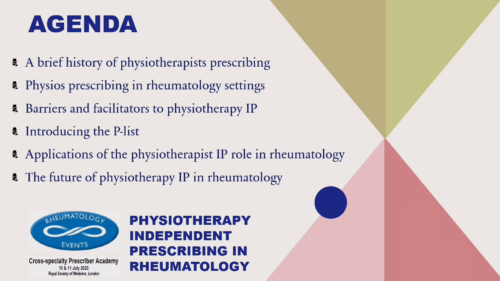
Presented by: Mr William Gregory (Consultant Physiotherapist, Salford Royal Hospital)Learning Objectives
A brief history of physiotherapist independent prescribing. Physiotherapists prescribing in rheumatology settings. Barriers and facilitators to physiotherapy independent prescribing Introducing the P-list. Applications of the physiotherapist independent prescribing role in rheumatology. The future of physiotherapy independent prescribing in rheumatology. -
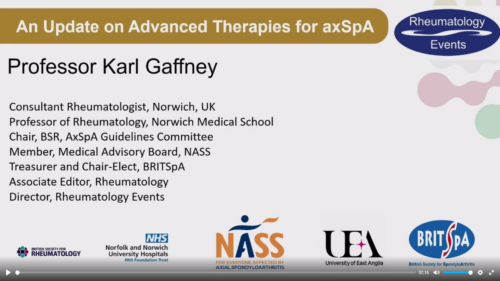

Presented by: Professor Karl Gaffney
Learning Objectives
Background: what is axial spondyloarthritis (axSpA)? Treatment goals in axSpA. The treatment landscape. Review of current therapy options. Switching after inadequate response to a medication. New therapies. Horizon scan of future treatments in axSpA. -

Presented by: Fomba Kallon (Clinical Nurse Specialist & Endoscopist in IBD, Chelsea & Westminster)
Learning Objectives
A clinical overview of inflammatory bowel disease for the non-gastroenterology specialist. The role of early and effective intervention. Empowering patients to manage their inflammatory bowel disease. Considering disease-, therapy- and individual patient-related factors. The roles and responsibilities of a clinical nurse specialist in inflammatory bowel disease. Training and practising as a clinical nurse endoscopist. Training and practising as a clinical nurse prescriber. -
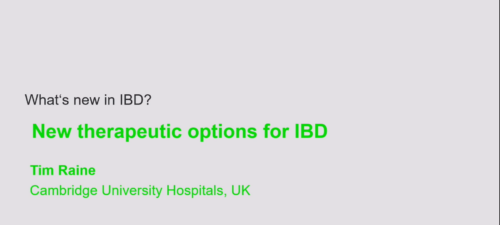
 Presented by: Dr Tim Raine (Consultant Gastroenterologist, Cambridge University Hospitals)
Presented by: Dr Tim Raine (Consultant Gastroenterologist, Cambridge University Hospitals)Learning Objectives
Emerging biologic and small molecule therapies for Crohn’s disease. Emerging biologic and small molecule therapies for ulcerative colitis. Safety of these emerging treatments. The gastrointestinal microbiome. Future treatment for inflammatory bowel disease. Considerations when co-managing patients with inflammatory bowel disease, arthritis, skin and/or eye disease. -
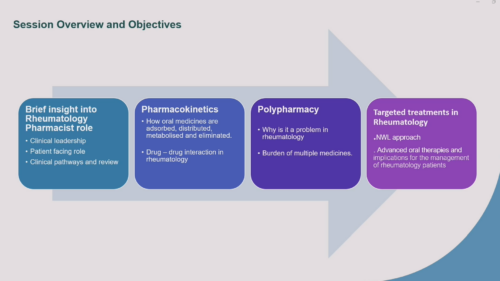

Presented by: Ms Kalveer Flora (Lead Rheumatology Specialist Pharmacist, London North West University NHS Healthcare)
Learning Objectives
Overview of the rheumatology pharmacist role, including: clinical leadership; patient-facing role; and clinical pathways and review. Pharmacokinetics: How oral medicines are absorbed, distributed, metabolised and eliminated. Drug-drug interactions in rheumatology. Polypharmacy: why is it a problem and it consequent burden. Targeted treatments in rheumatology: new approached to care with oral agents.